1 / 9
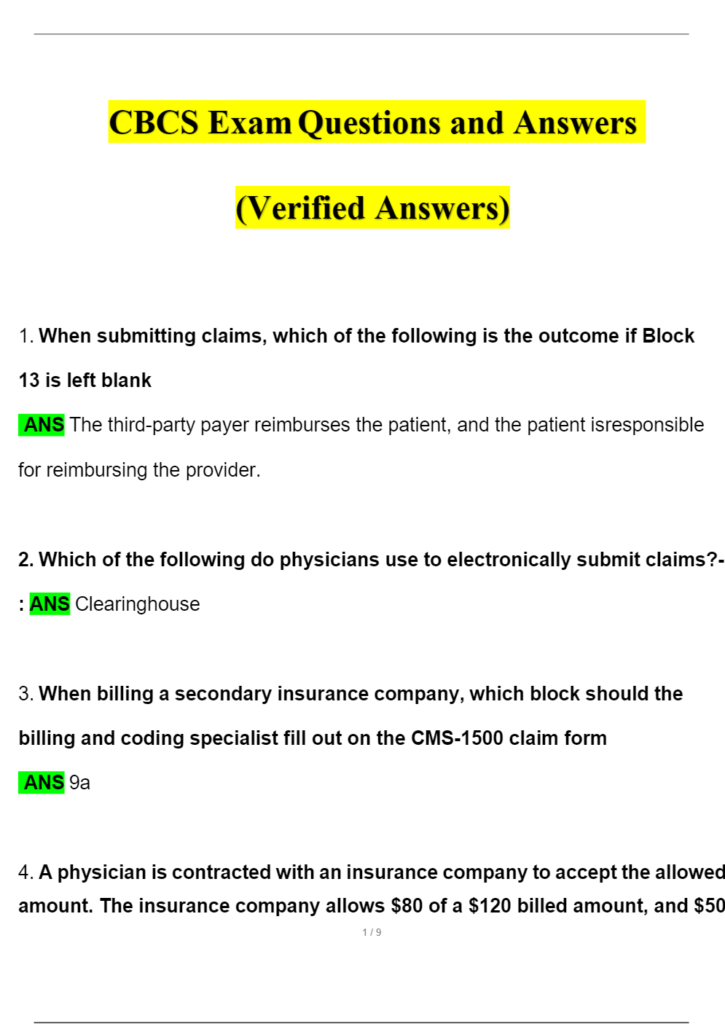
CBCS Exam Questions and Answers
(Verified Answers)
- When submitting claims, which of the following is the outcome if Block
13 is left blank
ANS The third-party payer reimburses the patient, and the patient isresponsible
for reimbursing the provider. - Which of the following do physicians use to electronically submit claims?-: ANS Clearinghouse
- When billing a secondary insurance company, which block should the
billing and coding specialist fill out on the CMS-1500 claim form
ANS 9a - A physician is contracted with an insurance company to accept the allowedamount. The insurance company allows $80 of a $120 billed amount, and $50
2 / 9
of the deductible has not been met. How much should the physician write offthe patient’s account ANS 40 - Which of the following is a requirement of some third-party payers before aprocedure is performed
ANS Preauthorization form - A dependent child whose parents both have insurance coverage comes tothe clinic.The billing and coding specialist uses the birthday rule to determinewhich insurance policy is primary.Which of the following describes the birthday rule
ANS The parent whose birthdate comes first in the calendar year - A prospective billing account audit prevents fraud by reviewing and comparing a completed claim form with which of the following documents
ANS A billing worksheet from the patient account - Which of the following documents is required to disclose an adult patient’sinformation
3 / 9
ANS A signed release from the patient
- After reading a provider’s notes about a new patient, a coding specialist
decides to code for a longer length of time than the actual office visit.Which
of the following describes the specialist’s action
ANS fraud - Two providers from the same practice visit a patient in the emergency
department using the same CPT code.The claim may be denied due to whichof the following reasons
ANS Duplication of services - The physician bills $500 to a patient. After submitting the claim to the insurance company, the claim is sent back with no payment.The patient still owes$500 for the year.This amount is called which of the following
ANS Deductible
get pdf at ;https://learnexams.com/search/study?query=